Throbbing Tooth Pain and Eye Swelling — Rare Sinus Carcinoma Uncovered
Patient Profile
45 Manhattan Beach resident with throbbing tooth pain worsening in mornings and eye swelling
Clinical Challenge
Advanced molar deterioration with CBCT revealing irregular bone borders, cortical plate involvement, and possible rare sinus carcinoma
Approach
CBCT-guided assessment followed by phased endodontic opening and CaOH medication to evaluate healing potential
Outcome
Tooth failed to heal, leading to extraction and biopsy confirming rare maxillary sinus carcinoma for targeted management
The Case
The patient, a 45-year-old Manhattan Beach resident, presented with throbbing pain in an upper molar that peaked every morning and was accompanied by noticeable swelling around the eye. Over-the-counter pain medications weren't touching it. The pain would ease somewhat as the day went on, but it never fully resolved.
History and Prior Treatment
The referring dentist had noted an abscess and prescribed a 10-day course of antibiotics, which the patient completed. A neighboring tooth had been extracted in January 2023. Despite the antibiotics, the symptoms persisted. On examination, we found a 6+ mm probing pocket on the distal aspect of the molar — deep enough to raise concern, but the real story was on the CBCT.
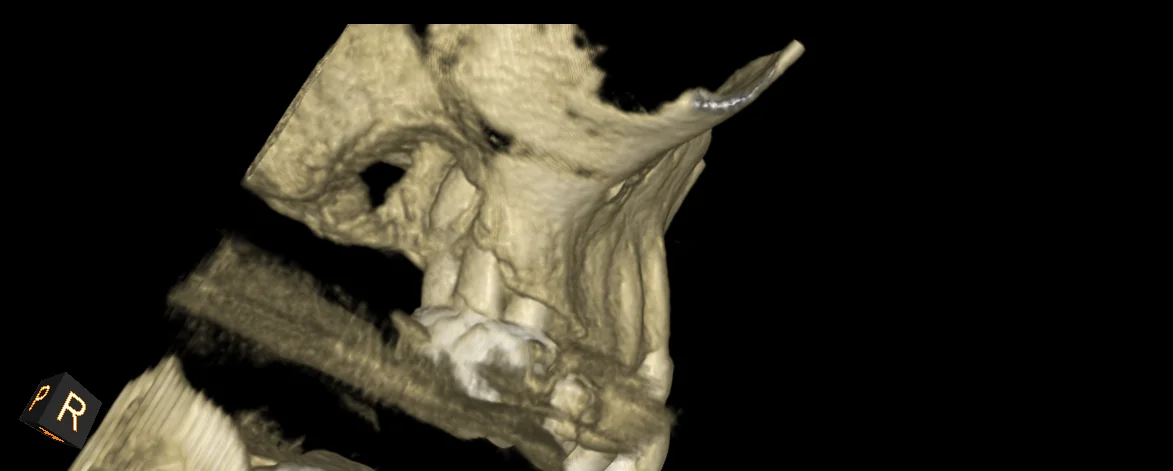
What the CBCT Showed
The 3D imaging revealed several findings that didn't fit a routine endo-perio presentation: calcification within the canal, furcation involvement, and — most concerning — irregular bone borders with cortical plate erosion. The borders weren't smooth the way you'd expect with a standard infection or cyst. They were ragged and ill-defined, which in rare cases can indicate malignancy.
Our Decision
Rather than rushing to extract, we opened the tooth and placed calcium hydroxide medication. The goal was to give the tooth a chance to respond to treatment. If it healed, we'd have our answer. If it didn't, the non-healing pattern combined with the imaging findings would justify extraction and biopsy for a definitive diagnosis.
Why This Mattered
This case is a reminder that not everything that looks like a dental infection is one. The combination of morning-dominant pain, eye swelling, and CBCT findings that didn't match a typical infection pattern told us something else was going on.
Why We Didn't Extract Immediately
It would have been easy to pull the tooth at the first visit. But without a clear diagnosis, extraction alone could have delayed the real answer. By medicating first, we created a diagnostic test: if the tooth responded to calcium hydroxide, the problem was likely infection. If it didn't, we had stronger justification for extraction with biopsy — and the patient understood exactly why.
The Differential Diagnosis
Our working differential included a combined endo-perio lesion, a vertical root fracture, and — given the irregular CBCT borders — possible maxillary sinus carcinoma. Sinus malignancies account for less than 0.2% of maxillary sinus pathologies, but the cortical plate erosion pattern on this CBCT was not something we could ignore.
The Outcome
The tooth did not respond to medication. We proceeded with extraction and sent the specimen for biopsy, which confirmed maxillary sinus carcinoma. The patient was referred to oncology promptly. Taking the phased approach meant we had a confirmed histological diagnosis before the patient entered cancer treatment — far better than discovering it incidentally months later.
Key Takeaways
Clinical Insights
- Irregular CBCT Borders Are a Red Flag: Smooth, well-defined radiolucencies suggest infection or cysts. Ragged, ill-defined borders with cortical plate erosion should raise suspicion for malignancy and warrant further investigation.
- Phased Treatment Serves as a Diagnostic Tool: Placing calcium hydroxide and monitoring response gives you information. Non-healing after conservative treatment strengthens the case for extraction and biopsy.
- 2D Radiographs Can Be Deceiving: The periapical radiograph in this case appeared relatively normal. Without CBCT, the irregular bone destruction pattern would have been missed entirely.
- Eye Swelling with Dental Pain Needs Advanced Workup: When symptoms extend beyond the tooth — especially to the orbit — the differential must include sinus pathology, not just dental infection.
When to Refer
- Persistent pain and swelling that don't resolve after antibiotics.
- CBCT showing irregular or ill-defined bone borders around the tooth apex or sinus floor.
- Non-healing after adequate endodontic intervention.
- Symptoms involving adjacent structures like the eye or cheek beyond typical dental presentation.
Bottom Line: A phased, CBCT-guided approach turned what could have been a routine extraction into a timely cancer diagnosis. Slowing down and letting the clinical picture develop gave this patient the best possible outcome.
Clinical Disclaimer: These cases are presented for educational purposes and published with appropriate patient consent. Patient identifying information has been removed in compliance with HIPAA regulations. Individual results may vary. All radiographic images and case descriptions represent actual patient treatment outcomes.
Procedures We Use for These Cases
The expertise demonstrated in these cases comes from mastering advanced endodontic procedures
CBCT 3D Imaging in Torrance
Cone beam CT 3D imaging in Torrance for precise endodontic diagnosis. See hidden canals, fractures & infections traditional X-rays miss. Call (310) 378-8342.
Learn moreEndodontic Consultation in Torrance, CA
Get a thorough endodontic consultation and dental pain diagnosis in Torrance. Dr. Jason Phan uses CBCT 3D imaging to find the real cause of your tooth pain.
Learn moreRelated Articles
Learn more about these treatments from Dr. Phan
 Cracked Teeth
Cracked Teeth Cracked Tooth: Crown, Root Canal, or Extraction? How We Decide
Not all cracked teeth need the same treatment. Dr. Jason Phan explains the 5 types of cracks, which ones can be saved, and how a microscope and CBCT determine the right treatment.
 Surgery & Retreatment
Surgery & Retreatment Failed Root Canal: Should You Try Retreatment or Get an Implant?
Your root canal didn't work — now what? Dr. Jason Phan compares retreatment vs. extraction and implant: success rates, costs, timelines, and how to decide which is right for your tooth.
 Root Canal
Root Canal Root Canal vs. Implant: Which Is the Better Investment for Your Tooth?
Choosing between saving your tooth with a root canal or extracting and replacing it with an implant? Dr. Jason Phan compares cost, success rates, timelines, and long-term outcomes.
 Root Canal
Root Canal Persistent Pain After Root Canal: Causes, Evidence, and When Retreatment Is Needed
A detailed clinical guide to understanding why pain persists after root canal treatment. Dr. Jason Phan covers odontogenic and nonodontogenic causes, diagnostic approaches, and evidence from current research.
 Consultation
Consultation What Happens During an Endodontic Consultation
Nervous about seeing an endodontist? Dr. Jason Phan walks you through exactly what happens during a consultation at our Torrance office — from the exam to the treatment plan.
 Pain Diagnosis
Pain Diagnosis Bruxism Pain Mimicking Root Canal Pain: When Grinding Feels Like a Toothache
Teeth grinding and clenching can cause tooth pain that mimics root canal symptoms. Dr. Jason Phan explains how a CBCT consultation in Torrance prevents unnecessary treatment.
 Pain Diagnosis
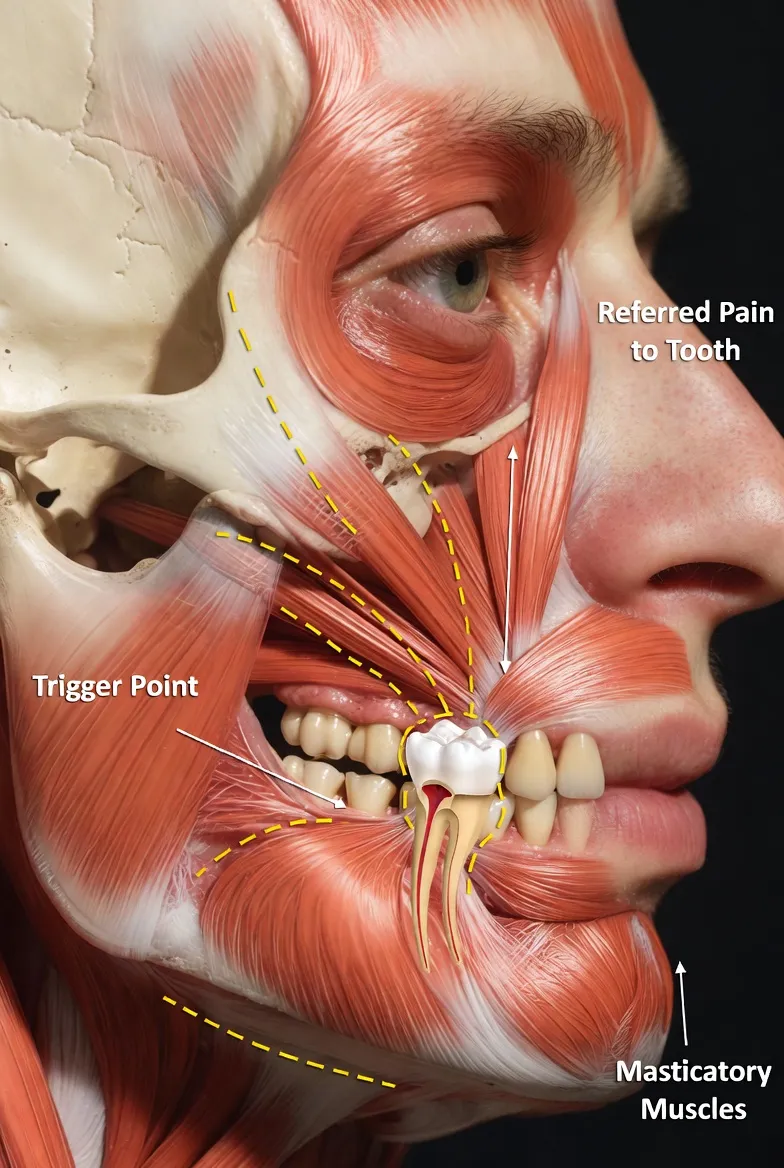
Pain Diagnosis Myofascial Pain Mimicking Root Canal Pain: When Jaw Muscles Cause Toothaches
Jaw muscle trigger points can refer pain to teeth, mimicking a root canal problem. Dr. Jason Phan explains how a detailed CBCT consultation in Torrance prevents misdiagnosis.
 Pain Diagnosis
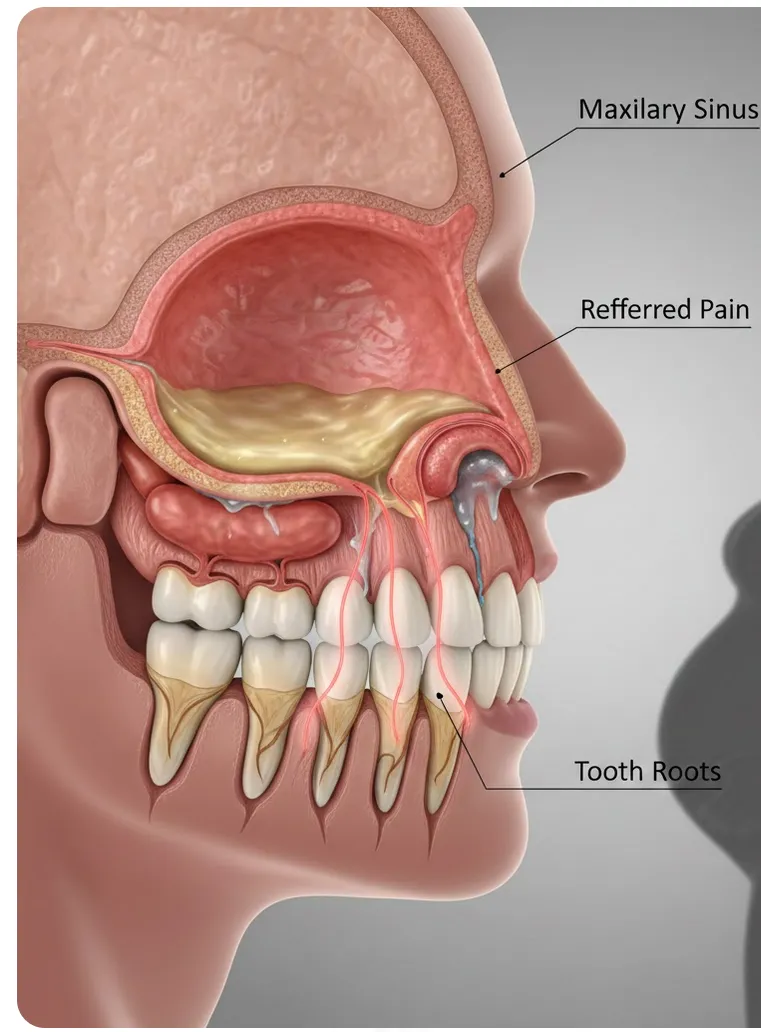
Pain Diagnosis Sinus Pain Mimicking Root Canal Pain: How to Tell the Difference
Maxillary sinusitis can cause tooth pain that feels like a root canal is needed. Dr. Jason Phan explains how CBCT imaging and thorough evaluation in Torrance prevent misdiagnosis.
 Pain Diagnosis
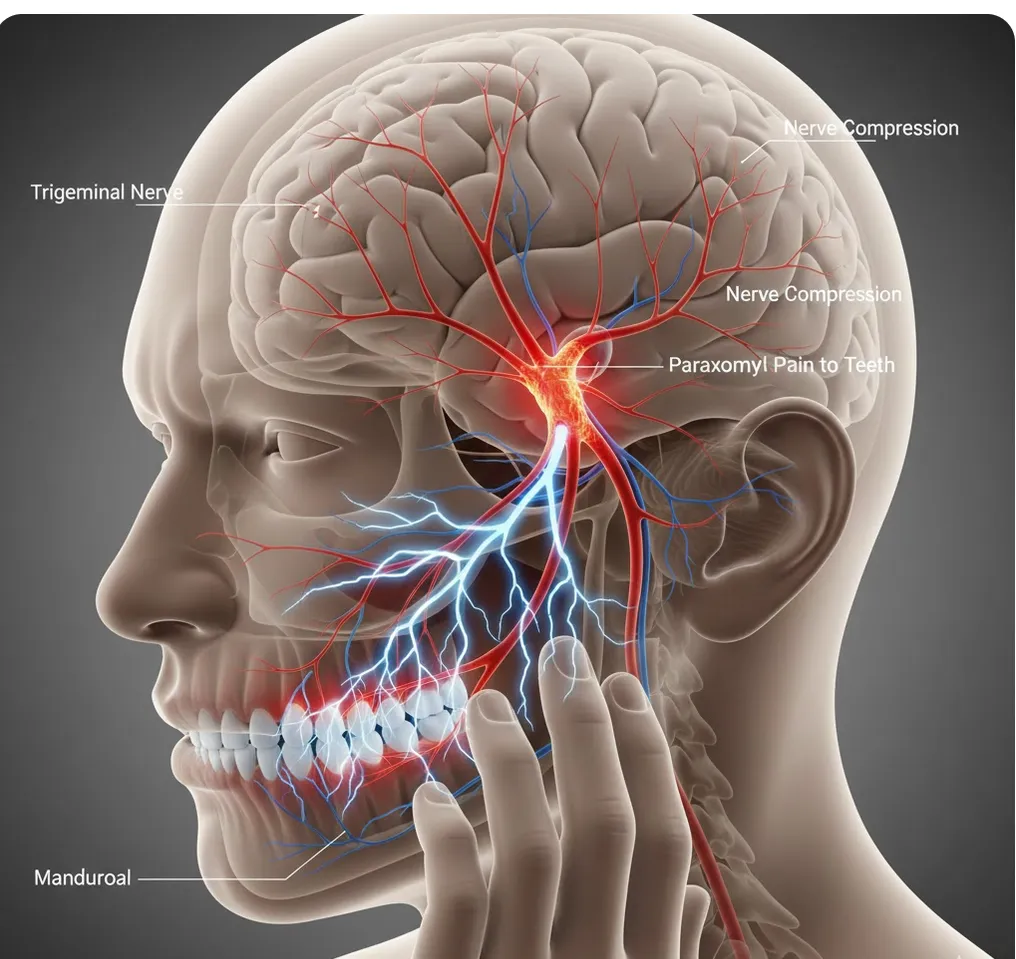
Pain Diagnosis Trigeminal Neuralgia & Other Nerve Conditions Mimicking Root Canal Pain
Trigeminal neuralgia causes intense facial pain often misdiagnosed as tooth problems. Dr. Jason Phan explains how CBCT consultation in Torrance prevents unnecessary root canals.
 Root Canal
Root Canal Endodontist vs. Dentist for Root Canal: 95% vs. 85% Success Rate
Endodontists have a 95–97% root canal success rate vs. 85–90% for general dentists. See the full comparison of training, equipment, cost, and when the specialist difference matters most.
 Pain Diagnosis
Pain Diagnosis Shingles Presenting as Tooth Pain: What You Need to Know
Shingles can mimic tooth pain, leading to unnecessary dental procedures. Dr. Jason Phan explains how herpes zoster affects the trigeminal nerve, the signs to watch for, and when to seek treatment.
Experience Matters in Complex Endodontics
When you refer patients to us, they benefit from decades of experience with the most challenging cases. We're here to help when routine endodontics isn't enough.
Mon-Fri: 8am-5pm | 23451 Madison St., Suite 210, Torrance, CA