Endo-Perio Lesion — Combined Infection Treatment Case

Patient Profile
34-year-old Hermosa Beach resident with deep 9mm pocket on distal of maxillary first molar, persistent pain and swelling
Clinical Challenge
Combined endodontic and periodontal pathology—difficult to determine primary etiology and sequence treatment appropriately
Approach
Endodontic treatment first to eliminate pulpal infection, followed by periodontal re-evaluation and possible surgical intervention
Outcome
Pocket reduced from 9mm to 4mm after endodontic treatment alone. Tooth stable at 8 year follow-up without periodontal surgery
Treatment Details
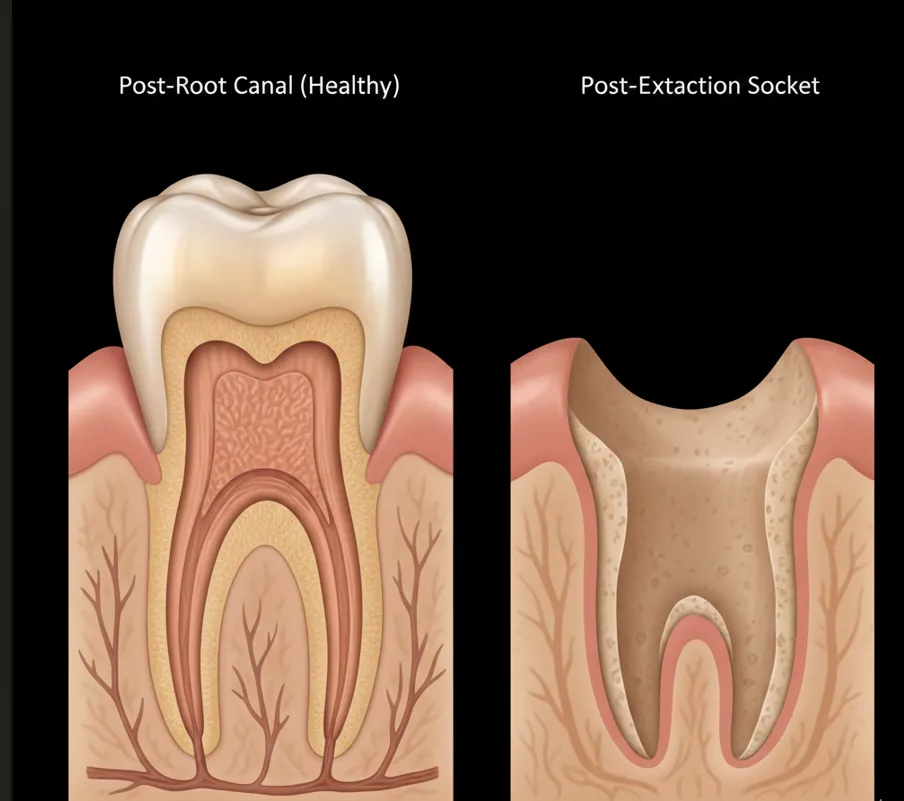
Combined endo-perio lesions represent one of the most challenging diagnostic and treatment scenarios in dentistry. The patient presented with a 9mm pocket on the distal of tooth #14, purulent exudate, and a large periapical radiolucency. Two questions needed answering: (1) Is this primarily an endodontic problem with secondary periodontal involvement, or vice versa? (2) What's the appropriate treatment sequence?
The diagnostic key was recognizing that the pocket communicated directly with the apex—classic for an endo-perio lesion originating from pulpal necrosis. Necrotic pulp tissue drains through the periodontal ligament, creating a pathway that mimics periodontal disease but has an endodontic origin.
Treatment Protocol
- Phase 1 - Endodontic Treatment: Complete cleaning and obturation of all root canals to eliminate pulpal infection source
- Phase 2 - Observation Period: 3-month waiting period to allow tissue response
- Phase 3 - Periodontal Re-evaluation: Reprobe pocket depths after endodontic healing
- Phase 4 - Periodontal Surgery (if needed): Only performed if pockets persist after endodontic healing
Why Sequence Matters
Performing periodontal surgery before addressing the endodontic infection wastes time and money. If the pocket is endodontic in origin, it will heal spontaneously once the canal is treated. In this case, the 9mm pocket reduced to 4mm within three months of endodontic therapy alone—no periodontal surgery required.
Technical Approach
- Thorough Canal Debridement: GentleWave irrigation essential for cleaning infected canals
- Calcium Hydroxide Medicament: Placed for 2 weeks to disinfect canal system
- Complete Obturation: Three-dimensional filling to seal canal and prevent reinfection
- Conservative Periodontal Therapy: Scaling and root planing performed after endodontic treatment
Clinical Assessment
This case demonstrates the critical importance of correct diagnosis in combined endo-perio cases. The literature is clear: treat the endodontic infection first, then re-evaluate. Patients and referring dentists sometimes push for immediate periodontal surgery, but this approach often fails because it addresses the secondary problem while leaving the primary infection untreated.
Classification of Endo-Perio Lesions
- Primary Endodontic: Pulpal necrosis with drainage through PDL (this case)—heals with endo alone
- Primary Periodontal: Periodontal disease exposing lateral/accessory canals—needs perio surgery
- True Combined: Independent endo and perio diseases—needs both treatments
Prognostic Assessment
At 8 year follow-up, this tooth demonstrates excellent healing:
- Pocket depth reduced from 9mm to 4mm (clinically healthy)
- Radiographic bone regeneration visible around apex
- No symptoms, no swelling, no mobility
- Tooth fully functional in occlusion
Had we performed periodontal surgery first, the patient would have undergone unnecessary surgical trauma with likely poor results since the infection source (necrotic pulp) would have remained untreated.
When Periodontal Surgery IS Needed
Indications for periodontal surgery after endodontic treatment:
- Pockets >5mm persist 3-6 months after successful endodontic therapy
- Furcation involvement remains despite canal treatment
- Vertical bone defects don't show regeneration
- True primary periodontal disease coexists with endodontic pathology
Key Takeaways
Clinical Insights
- Treat endo first, always: Even when periodontal involvement looks severe, endodontic treatment must come first. Re-evaluate pockets after 3-6 months of healing.
- Most "endo-perio" lesions are primarily endodontic: About 70% of deep pockets associated with periapical lesions will heal with endodontic treatment alone.
- Patience prevents unnecessary surgery: Giving tissues time to heal after canal treatment often eliminates the need for periodontal surgery.
- Radiographic healing lags clinical healing: Pockets improve faster than radiographs. Don't judge success solely on X-rays.
- Communication with periodontists is essential: Coordinate treatment sequencing to avoid redundant or premature procedures.
Diagnostic Clues for Primary Endodontic Lesions
- Isolated deep pocket with no generalized periodontal disease
- Pocket probes directly to apex of tooth
- Necrotic pulp on testing (no response to cold)
- Radiographic periapical lesion continuous with pocket
- No calculus or heavy deposits in the deep pocket
Bottom Line: When you see deep pockets with periapical radiolucencies, assume endodontic origin until proven otherwise. Treat the canals first, wait 3-6 months, then reassess. This conservative approach saves most teeth and prevents unnecessary periodontal surgery.
Clinical Disclaimer: These cases are presented for educational purposes and published with appropriate patient consent. Patient identifying information has been removed in compliance with HIPAA regulations. Individual results may vary. All radiographic images and case descriptions represent actual patient treatment outcomes.
Procedures We Use for These Cases
The expertise demonstrated in these cases comes from mastering advanced endodontic procedures
Abscess & Emergency Tooth Care in Torrance, CA
Same-day emergency abscess tooth treatment in Torrance. Dr. Jason Phan drains infections, manages pain, and saves teeth. Call (310) 378-8342 now.
Learn moreGentleWave Root Canal in Torrance
GentleWave root canal cleaning in Torrance removes 95%+ bacteria using fluid dynamics. Preserves tooth structure. Call (310) 378-8342.
Learn moreRelated Articles
Learn more about these treatments from Dr. Phan
 Root Canal
Root Canal GentleWave vs. Traditional Root Canal: Is the Upgrade Worth It?
GentleWave removes 95%+ bacteria vs. 40–60% with traditional files. Dr. Jason Phan explains how it works, what it costs, who benefits most, and whether insurance covers it.
 Root Canal
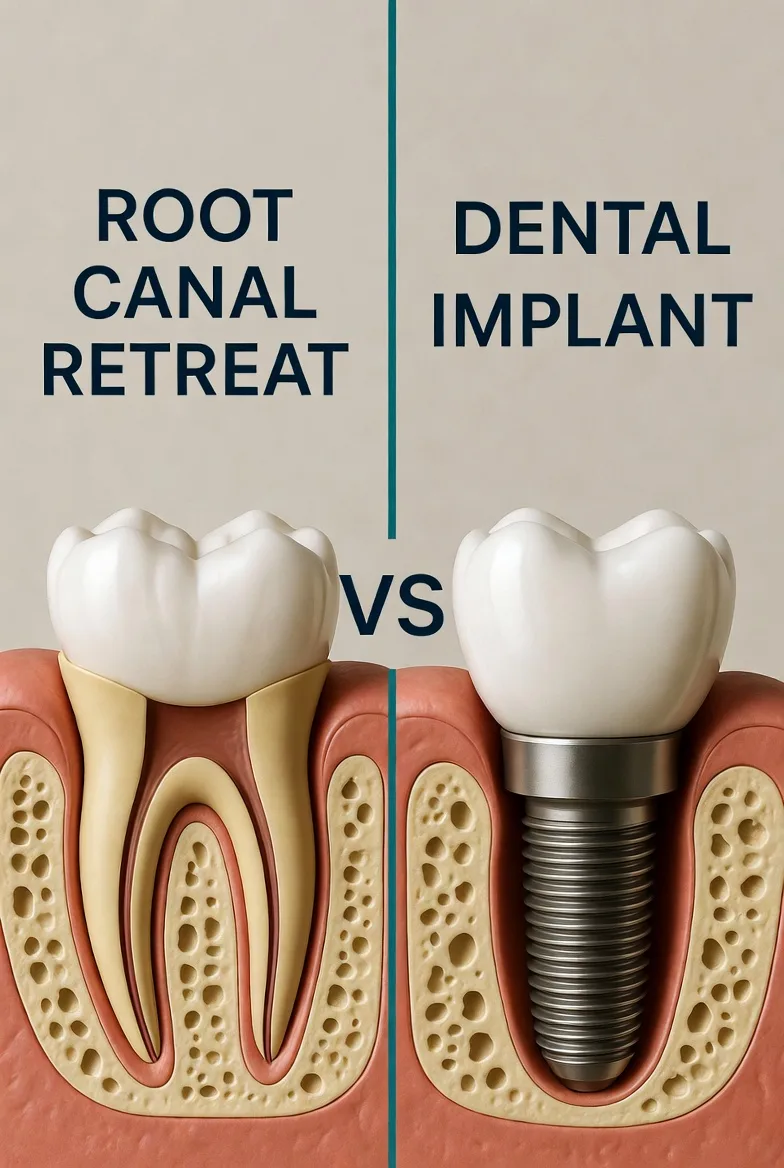
Root Canal Root Canal vs. Implant: Which Is the Better Investment for Your Tooth?
Choosing between saving your tooth with a root canal or extracting and replacing it with an implant? Dr. Jason Phan compares cost, success rates, timelines, and long-term outcomes.
 Root Canal
Root Canal Persistent Pain After Root Canal: Causes, Evidence, and When Retreatment Is Needed
A detailed clinical guide to understanding why pain persists after root canal treatment. Dr. Jason Phan covers odontogenic and nonodontogenic causes, diagnostic approaches, and evidence from current research.
 Root Canal
Root Canal Why Does My Tooth Still Hurt After a Root Canal?
Worried about lingering pain after root canal treatment? Dr. Jason Phan explains what's normal, what's not, and when it's time for a specialist evaluation.
 Root Canal
Root Canal What Is Internal Tooth Bleaching After a Root Canal?
Got a dark tooth after a root canal? Dr. Jason Phan explains internal bleaching — a simple procedure that whitens your tooth from the inside out without a veneer or crown.
 Surgery & Retreatment
Surgery & Retreatment Root Canal Retreatment: When Your First Root Canal Fails
Your root canal didn't work. Now what? Dr. Jason Phan explains why root canals fail, what retreatment involves, and when it's worth saving the tooth.
 Emergency & Abscess
Emergency & Abscess Tooth Abscess Emergency: What to Do Before Your Appointment
A dental abscess won't wait. Dr. Jason Phan explains what a tooth abscess is, what to do at home before you can get in, and why you shouldn't ignore the swelling.
 Root Canal
Root Canal Root Canal Pain After Treatment: What's Normal and What's Not
Some discomfort after a root canal is normal, but how do you know if something is wrong? Dr. Jason Phan explains what to expect during recovery, warning signs to watch for, and when to call your endodontist.
 Root Canal
Root Canal Root Canal or Extraction: How to Decide What's Best for Your Tooth
Should you save your tooth with a root canal or have it pulled? Dr. Jason Phan compares outcomes, costs, recovery, and long-term consequences to help you make the right decision.
 Root Canal
Root Canal Endodontist vs. Dentist for Root Canal: 95% vs. 85% Success Rate
Endodontists have a 95–97% root canal success rate vs. 85–90% for general dentists. See the full comparison of training, equipment, cost, and when the specialist difference matters most.
 Root Canal
Root Canal How Much Does a Root Canal Cost Without Insurance?
Root canal costs without insurance typically range from $1,300 to $2,000. Dr. Jason Phan breaks down what affects pricing, how it compares to extraction and implants, and affordable payment options.
 Root Canal
Root Canal Root Canal Recovery: What to Expect After Treatment
A complete guide to root canal recovery. Dr. Jason Phan explains what's normal, how to manage discomfort, and when to call the office after your procedure.
 Root Canal
Root Canal 7 Signs You Might Need a Root Canal
Not sure if you need a root canal? Dr. Jason Phan explains the warning signs of tooth infection—from persistent pain to gum swelling—and when to seek treatment.
 Root Canal
Root Canal 5 Root Canal Myths Debunked by a Torrance Endodontist
Dr. Jason Phan separates fact from fiction about root canal treatment. Learn the truth about pain, safety, and what to really expect from modern endodontic care.
Experience Matters in Complex Endodontics
When you refer patients to us, they benefit from decades of experience with the most challenging cases. We're here to help when routine endodontics isn't enough.
Mon-Fri: 8am-5pm | 23451 Madison St., Suite 210, Torrance, CA