Calcified Root Canal Treated with CBCT and GentleWave
Patient Profile
45-year-old male referred from his Manhattan Beach dentist with persistent pain in previously treated maxillary first molar
Clinical Challenge
Severely calcified MB2 canal not located during initial treatment—CBCT showed complete sclerosis
Approach
CBCT-guided access, ultrasonic troughing, micro-openers, GentleWave multisonic irrigation
Outcome
MB2 canal successfully negotiated, cleaned, and obturated. Patient asymptomatic at 2-year follow-up
Treatment Details
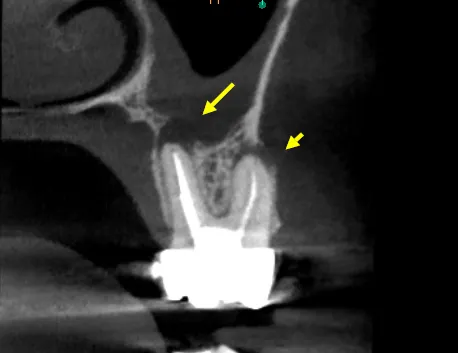
The referring dentist had completed what appeared to be adequate endodontic treatment two years prior, but the patient continued to experience intermittent discomfort and sensitivity to percussion. Clinical examination revealed no obvious defects, but CBCT imaging told a different story: a completely calcified MB2 canal with associated periapical pathology.
Calcification of this severity requires a systematic approach. We used CBCT data to precisely locate the canal orifice, then employed ultrasonic tips to create a troughing pathway through the sclerotic dentin. Micro-openers (size 06 and 08) were used to negotiate the calcified canal under high magnification.
Technical Protocol
- CBCT Analysis: Identified exact MB2 location and depth of calcification
- Microscope Magnification: 16x magnification for precise visualization
- Ultrasonic Troughing: CPR tips to remove calcified dentin shelf
- Micro-Opener Files: Negotiated sclerotic canal to working length
- GentleWave Irrigation: Multisonic cleaning of complex anatomy
- Warm Vertical Compaction: Three-dimensional obturation of all canals
The entire procedure took approximately 2 hours. The canal was successfully negotiated to full working length, cleaned with GentleWave technology, and obturated along with the other three canals.
Clinical Assessment
This case represents the type of challenge that defines specialist endodontic care. The MB2 canal in maxillary first molars is present in approximately 95% of teeth, yet it's frequently missed during routine treatment—not due to negligence, but because of calcification that makes it invisible without advanced imaging and magnification.
At 2-year follow-up, the patient remains completely asymptomatic with radiographic evidence of periapical healing. The tooth is functional and the patient reports no sensitivity.
Why This Case Required Specialist Referral
- CBCT Integration: Essential for locating calcified anatomy invisible on 2D radiographs
- Surgical Microscope: High magnification (16x-25x) required for visualization
- Specialized Instruments: Ultrasonic tips and micro-openers not typically available in general practice
- Time Investment: Two hours of focused specialist attention
- Experience Factor: Pattern recognition from treating hundreds of calcified canals
General dentists appropriately refer these cases because the alternative—leaving the infected canal untreated—leads to continued pathology and eventual tooth loss.
Key Takeaways
Clinical Insights
- MB2 is almost always there: If you can't find it, assume it's calcified rather than absent. CBCT will reveal the truth.
- Calcification patterns are predictable: With experience, you learn where to look and how deep to trough. It's not guesswork.
- Technology enables success: This case was impossible 15 years ago. CBCT, microscopes, and ultrasonics transformed outcomes.
- Patience is non-negotiable: Rushing through calcified canals leads to perforations. Slow, methodical troughing is the only safe approach.
- GentleWave matters in calcified cases: Traditional irrigation can't penetrate sclerotic canals. Multisonic technology reaches areas that needles cannot.
When to Refer Calcified Canal Cases
Consider specialist referral when:
- Radiographs show no visible canal space in symptomatic teeth
- Canals cannot be negotiated after reasonable attempts
- CBCT reveals anatomy that's invisible on periapical films
- Patient's symptoms persist despite apparently adequate treatment
- MB2 cannot be located in maxillary molars with periapical pathology
Bottom Line: Calcified canals are solvable problems, but they require specialized training, equipment, and time that most general practices cannot provide. Early referral prevents months of patient discomfort.
Clinical Disclaimer: These cases are presented for educational purposes and published with appropriate patient consent. Patient identifying information has been removed in compliance with HIPAA regulations. Individual results may vary. All radiographic images and case descriptions represent actual patient treatment outcomes.
Procedures We Use for These Cases
The expertise demonstrated in these cases comes from mastering advanced endodontic procedures
CBCT 3D Imaging in Torrance
Cone beam CT 3D imaging in Torrance for precise endodontic diagnosis. See hidden canals, fractures & infections traditional X-rays miss. Call (310) 378-8342.
Learn moreGentleWave Root Canal in Torrance
GentleWave root canal cleaning in Torrance removes 95%+ bacteria using fluid dynamics. Preserves tooth structure. Call (310) 378-8342.
Learn moreRelated Articles
Learn more about these treatments from Dr. Phan
 Root Canal
Root Canal GentleWave vs. Traditional Root Canal: Is the Upgrade Worth It?
GentleWave removes 95%+ bacteria vs. 40–60% with traditional files. Dr. Jason Phan explains how it works, what it costs, who benefits most, and whether insurance covers it.
 Root Canal
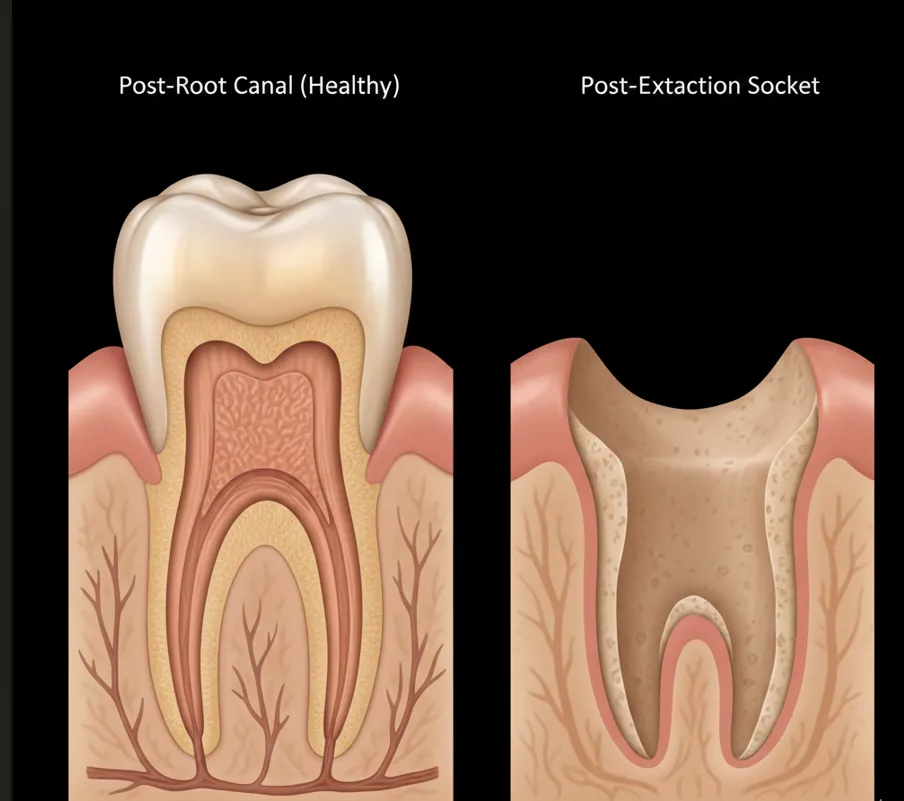
Root Canal Root Canal vs. Implant: Which Is the Better Investment for Your Tooth?
Choosing between saving your tooth with a root canal or extracting and replacing it with an implant? Dr. Jason Phan compares cost, success rates, timelines, and long-term outcomes.
 Root Canal
Root Canal Persistent Pain After Root Canal: Causes, Evidence, and When Retreatment Is Needed
A detailed clinical guide to understanding why pain persists after root canal treatment. Dr. Jason Phan covers odontogenic and nonodontogenic causes, diagnostic approaches, and evidence from current research.
 Root Canal
Root Canal Why Does My Tooth Still Hurt After a Root Canal?
Worried about lingering pain after root canal treatment? Dr. Jason Phan explains what's normal, what's not, and when it's time for a specialist evaluation.
 Root Canal
Root Canal What Is Internal Tooth Bleaching After a Root Canal?
Got a dark tooth after a root canal? Dr. Jason Phan explains internal bleaching — a simple procedure that whitens your tooth from the inside out without a veneer or crown.
 Surgery & Retreatment
Surgery & Retreatment Root Canal Retreatment: When Your First Root Canal Fails
Your root canal didn't work. Now what? Dr. Jason Phan explains why root canals fail, what retreatment involves, and when it's worth saving the tooth.
 Root Canal
Root Canal Root Canal Pain After Treatment: What's Normal and What's Not
Some discomfort after a root canal is normal, but how do you know if something is wrong? Dr. Jason Phan explains what to expect during recovery, warning signs to watch for, and when to call your endodontist.
 Root Canal
Root Canal Root Canal or Extraction: How to Decide What's Best for Your Tooth
Should you save your tooth with a root canal or have it pulled? Dr. Jason Phan compares outcomes, costs, recovery, and long-term consequences to help you make the right decision.
 Root Canal
Root Canal Endodontist vs. Dentist for Root Canal: 95% vs. 85% Success Rate
Endodontists have a 95–97% root canal success rate vs. 85–90% for general dentists. See the full comparison of training, equipment, cost, and when the specialist difference matters most.
 Root Canal
Root Canal How Much Does a Root Canal Cost Without Insurance?
Root canal costs without insurance typically range from $1,300 to $2,000. Dr. Jason Phan breaks down what affects pricing, how it compares to extraction and implants, and affordable payment options.
 Root Canal
Root Canal Root Canal Recovery: What to Expect After Treatment
A complete guide to root canal recovery. Dr. Jason Phan explains what's normal, how to manage discomfort, and when to call the office after your procedure.
 Root Canal
Root Canal 7 Signs You Might Need a Root Canal
Not sure if you need a root canal? Dr. Jason Phan explains the warning signs of tooth infection—from persistent pain to gum swelling—and when to seek treatment.
 Root Canal
Root Canal 5 Root Canal Myths Debunked by a Torrance Endodontist
Dr. Jason Phan separates fact from fiction about root canal treatment. Learn the truth about pain, safety, and what to really expect from modern endodontic care.
Experience Matters in Complex Endodontics
When you refer patients to us, they benefit from decades of experience with the most challenging cases. We're here to help when routine endodontics isn't enough.
Mon-Fri: 8am-5pm | 23451 Madison St., Suite 210, Torrance, CA