C-Shaped Canal Anatomy — Complex Root Canal Case

Patient Profile
51-year-old Gardena resident with severe pain in lower right second molar, no response to cold
Clinical Challenge
C-shaped canal configuration with continuous ribbon connecting all canal spaces—impossible to negotiate with standard techniques; tough restorative challenge
Approach
CBCT mapping, modified access cavity design, circumferential filing technique, GentleWave irrigation
Outcome
Complete debridement of C-shaped system, three-dimensional obturation, pain resolved immediately
Treatment Details
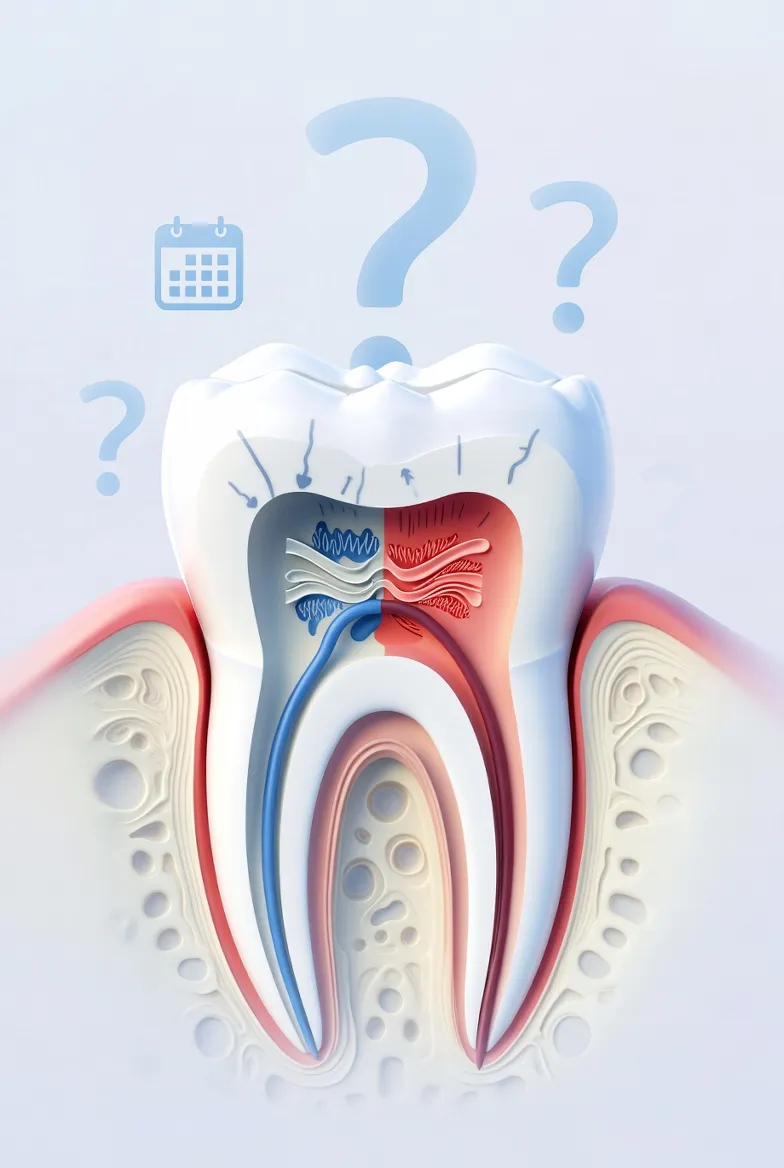
C-shaped canals occur in approximately 30-45% of mandibular second molars in certain populations, but they're rarely encountered by general dentists because the anatomical variation isn't visible on standard radiographs. This patient's CBCT revealed a Type I C-configuration—a continuous ribbon of pulp tissue connecting what would normally be separate mesial and distal canals.
Standard treatment protocols don't work for C-shaped anatomy. You cannot simply "find the canals" and file them independently because there are no discrete canals—just a continuous C-shaped space with isthmus connections throughout the entire root length.
Modified Treatment Protocol
- Access Modification: Trapezoidal cavity instead of traditional triangular to expose entire C-configuration
- Circumferential Filing: Rasping motion along the inner and outer walls of the C-shape rather than traditional filing
- Abundant Irrigation: GentleWave multisonic cleaning essential for reaching fins and isthmus areas
- Thermoplasticized Obturation: Warm vertical compaction to fill irregular three-dimensional anatomy
- Multiple Cone Technique: Several gutta-percha points placed to fill the ribbon-like space
The procedure took 90 minutes. The patient's severe pain resolved immediately after treatment.
Clinical Assessment
This case demonstrates why anatomical knowledge distinguishes specialist practice from routine dentistry. The referring dentist suspected "something unusual" based on the radiograph and wisely referred before attempting treatment. Had standard techniques been applied, the result would likely have been incomplete debridement and persistent infection.
Recognition is the Critical Skill
The key to managing complex anatomy is recognizing when you're dealing with it:
- Radiographs that show "merging" canals in mandibular molars suggest C-shaped anatomy
- Single large orifice when you expect to see two separate openings
- Inability to negotiate what appears to be a straight canal
- Bleeding from areas between canal orifices (indicates isthmus connections)
When these signs appear, CBCT imaging should be obtained before proceeding. Attempting to treat C-shaped canals without understanding the anatomy leads to incomplete cleaning and treatment failure.
Technology Requirements
- CBCT: Essential for visualizing the three-dimensional C-configuration
- Microscope: High magnification needed to see the ribbon-like anatomy
- Advanced Irrigation: Traditional syringe irrigation cannot clean these complex spaces
- Thermoplasticized Obturation: Cold lateral compaction inadequate for irregular shapes
Key Takeaways
Clinical Insights
- Anatomical variation is common: About 30% of lower second molars have unusual anatomy. It's not rare—it's just rarely recognized.
- Radiographs lie: Two-dimensional images cannot reveal three-dimensional ribbon-like anatomy. When something looks "weird," get CBCT before proceeding.
- Treatment protocols must adapt: Textbook techniques designed for "normal" anatomy fail in variant cases. You need different access, different filing, different irrigation.
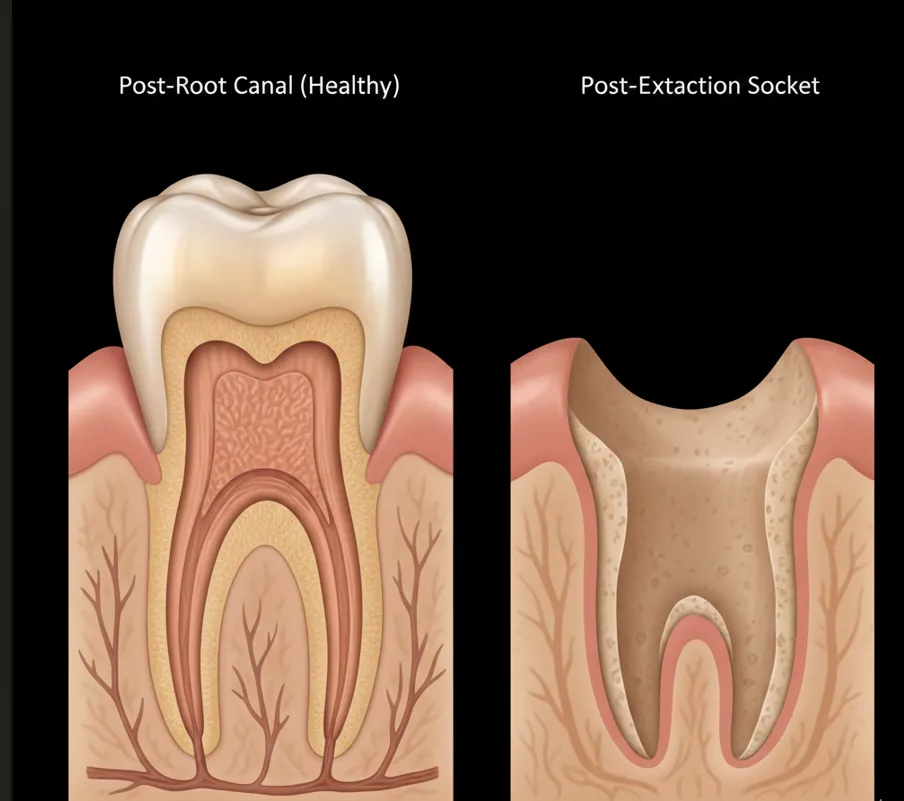
- Prevention is easier than repair: Treating C-shaped anatomy correctly the first time is far easier than attempting retreatment after failed standard therapy.
When to Suspect C-Shaped Anatomy
- Mandibular second molars (especially in Asian patients—genetic variation)
- Radiographs showing canal "merging" or unclear canal count
- Single large orifice instead of expected separate openings
- Difficulty negotiating apparently straight canals
- Persistent bleeding between canal orifices during access
Clinical Wisdom: When anatomy doesn't match your mental model, stop and reassess. CBCT is cheaper than retreatment.
Clinical Disclaimer: These cases are presented for educational purposes and published with appropriate patient consent. Patient identifying information has been removed in compliance with HIPAA regulations. Individual results may vary. All radiographic images and case descriptions represent actual patient treatment outcomes.
Procedures We Use for These Cases
The expertise demonstrated in these cases comes from mastering advanced endodontic procedures
CBCT 3D Imaging in Torrance
Cone beam CT 3D imaging in Torrance for precise endodontic diagnosis. See hidden canals, fractures & infections traditional X-rays miss. Call (310) 378-8342.
Learn moreGentleWave Root Canal in Torrance
GentleWave root canal cleaning in Torrance removes 95%+ bacteria using fluid dynamics. Preserves tooth structure. Call (310) 378-8342.
Learn moreRelated Articles
Learn more about these treatments from Dr. Phan
 Root Canal
Root Canal GentleWave vs. Traditional Root Canal: Is the Upgrade Worth It?
GentleWave removes 95%+ bacteria vs. 40–60% with traditional files. Dr. Jason Phan explains how it works, what it costs, who benefits most, and whether insurance covers it.
 Root Canal
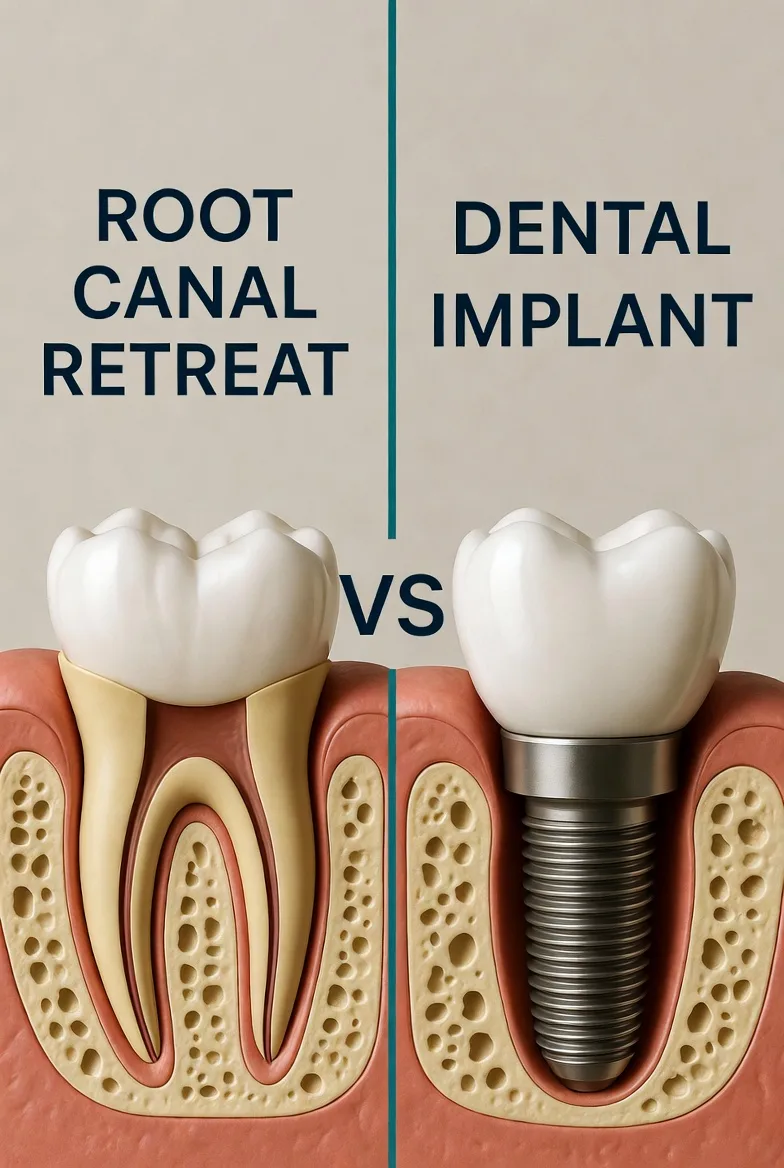
Root Canal Root Canal vs. Implant: Which Is the Better Investment for Your Tooth?
Choosing between saving your tooth with a root canal or extracting and replacing it with an implant? Dr. Jason Phan compares cost, success rates, timelines, and long-term outcomes.
 Root Canal
Root Canal Persistent Pain After Root Canal: Causes, Evidence, and When Retreatment Is Needed
A detailed clinical guide to understanding why pain persists after root canal treatment. Dr. Jason Phan covers odontogenic and nonodontogenic causes, diagnostic approaches, and evidence from current research.
 Root Canal
Root Canal Why Does My Tooth Still Hurt After a Root Canal?
Worried about lingering pain after root canal treatment? Dr. Jason Phan explains what's normal, what's not, and when it's time for a specialist evaluation.
 Root Canal
Root Canal What Is Internal Tooth Bleaching After a Root Canal?
Got a dark tooth after a root canal? Dr. Jason Phan explains internal bleaching — a simple procedure that whitens your tooth from the inside out without a veneer or crown.
 Surgery & Retreatment
Surgery & Retreatment Root Canal Retreatment: When Your First Root Canal Fails
Your root canal didn't work. Now what? Dr. Jason Phan explains why root canals fail, what retreatment involves, and when it's worth saving the tooth.
 Root Canal
Root Canal Root Canal Pain After Treatment: What's Normal and What's Not
Some discomfort after a root canal is normal, but how do you know if something is wrong? Dr. Jason Phan explains what to expect during recovery, warning signs to watch for, and when to call your endodontist.
 Root Canal
Root Canal Root Canal or Extraction: How to Decide What's Best for Your Tooth
Should you save your tooth with a root canal or have it pulled? Dr. Jason Phan compares outcomes, costs, recovery, and long-term consequences to help you make the right decision.
 Root Canal
Root Canal Endodontist vs. Dentist for Root Canal: 95% vs. 85% Success Rate
Endodontists have a 95–97% root canal success rate vs. 85–90% for general dentists. See the full comparison of training, equipment, cost, and when the specialist difference matters most.
 Root Canal
Root Canal How Much Does a Root Canal Cost Without Insurance?
Root canal costs without insurance typically range from $1,300 to $2,000. Dr. Jason Phan breaks down what affects pricing, how it compares to extraction and implants, and affordable payment options.
 Root Canal
Root Canal Root Canal Recovery: What to Expect After Treatment
A complete guide to root canal recovery. Dr. Jason Phan explains what's normal, how to manage discomfort, and when to call the office after your procedure.
 Root Canal
Root Canal 7 Signs You Might Need a Root Canal
Not sure if you need a root canal? Dr. Jason Phan explains the warning signs of tooth infection—from persistent pain to gum swelling—and when to seek treatment.
 Root Canal
Root Canal 5 Root Canal Myths Debunked by a Torrance Endodontist
Dr. Jason Phan separates fact from fiction about root canal treatment. Learn the truth about pain, safety, and what to really expect from modern endodontic care.
Experience Matters in Complex Endodontics
When you refer patients to us, they benefit from decades of experience with the most challenging cases. We're here to help when routine endodontics isn't enough.
Mon-Fri: 8am-5pm | 23451 Madison St., Suite 210, Torrance, CA