Intentional Reimplantation — Saving a Molar When Retreatment Fails
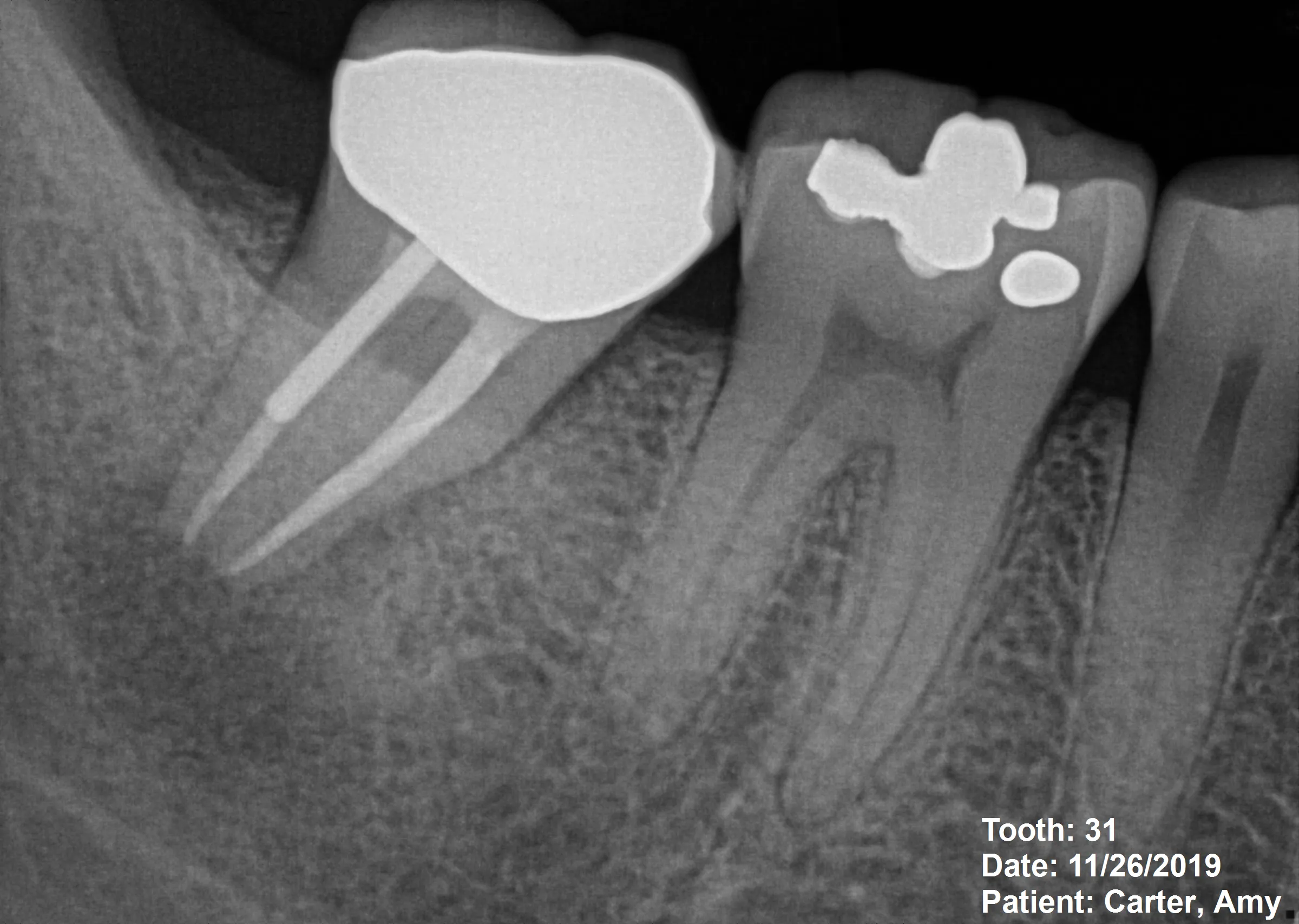
Patient Profile
54-year-old Palos Verdes patient with sudden severe pain in lower mandibular molar
Clinical Challenge
Previous root canal treatment failing, with large metallic post blocking orthograde access
Approach
Atraumatic extraction with ultrasonic apical preparation and MTA retrofill, followed by immediate reimplantation
Outcome
Symptoms resolved, tooth remains stable, with signs of bone regeneration
What is Intentional Reimplantation?
Intentional reimplantation is defined as the deliberate extraction of a tooth, followed by extraoral endodontic treatment and immediate reinsertion into its original socket. Once considered a "last resort" procedure, recent research shows it has evolved into a mainstream treatment option with success rates of 77-90% when proper case selection and technique are employed.
Modern Perspective
Recent studies published in 2024-2025 demonstrate a significant shift in clinical perception:
- 72.7% of endodontists now view intentional reimplantation as an adjunct treatment modality rather than a desperate last option
- Success rates of 88-95% reported in systematic reviews with proper technique
- Cost-effective alternative to extraction and implant placement, preserving natural tooth structure
- Predictable outcomes when case selection criteria are followed
Indications for Intentional Reimplantation
This procedure is appropriate when:
- Conventional nonsurgical retreatment is impossible or has failed
- Surgical endodontic access (apicoectomy) is impractical due to anatomy or proximity to vital structures
- Large posts or separated instruments block orthograde access
- Complex root anatomy makes conventional treatment unreasonable
- Patient desires natural tooth preservation over extraction/implant
- Tooth has adequate periodontal support and restorative prognosis
Contraindications
Intentional reimplantation should be avoided when:
- Teeth have severely flared, curved, or dilacerated roots (high extraction fracture risk)
- Vertically fractured teeth
- Non-restorable teeth with insufficient crown structure
- Advanced periodontal disease (two or more pockets ≥6mm)
- Medical conditions contraindicate extraction or surgery
Step-by-Step Protocol
Intentional reimplantation success depends on meticulous technique and minimizing extraoral time. Research demonstrates that survival decreases 1.7-fold when extraoral time exceeds 15 minutes, as prolonged drying damages the periodontal ligament cells critical for reattachment.
Preoperative Phase
- CBCT Imaging: Essential for evaluating root morphology, planning extraction approach, and identifying anatomical obstacles
- Patient Preparation: Chlorhexidine 0.12% rinse one hour before procedure; systemic antibiotics if indicated for high-risk cases
- Informed Consent: Discuss alternative treatments (extraction/implant), risk of root fracture during extraction, and possibility of root resorption
- Setup: Prepare all instruments before extraction—ultrasonic tips, MTA/bioceramic material, irrigation solutions—so tooth can be reimplanted within 15 minutes
Surgical Phase (Time-Critical)
- Atraumatic Extraction (Minutes 0-5):
- Use minimal luxation forces with elevators
- Gentle rotational movements with forceps
- Avoid aggressive rocking that may fracture roots
- Extract tooth cleanly, preserving as much PDL as possible on root surface
- Socket Management (During Extraoral Work):
- Irrigate socket with sterile saline to remove debris
- Preserve socket walls—do not curette aggressively
- Keep socket moist with saline-soaked gauze
- Extraoral Root-End Preparation (Minutes 5-12):
- Resect 3mm of root apex using high-speed handpiece or ultrasonic tip
- Prepare retrograde cavity using ultrasonic tips parallel to root long axis
- Cavity depth: 3mm minimum for adequate seal
- Inspect for cracks, fractures, or isthmuses under magnification
- Retrograde Seal (Minutes 12-14):
- Place bioceramic material (MTA or EndoSequence Root Repair Material)
- Ensure complete seal of apical anatomy including isthmuses
- Verify material adaptation with magnification
- Reimplantation (Minute 15):
- Irrigate socket with sterile saline immediately before reinsertion
- Gently seat tooth back into socket with firm digital pressure
- Verify positioning matches original position
- Check occlusion—tooth should not have premature contact
Postoperative Management
- Splinting: Flexible splint for 7-14 days (evidence varies; some studies show no splinting is acceptable)
- Radiograph: Immediate postoperative film to document position
- Medications: NSAIDs for pain management; antibiotics as indicated by patient risk factors
- Instructions: Soft diet for 2 weeks, avoid chewing on treated tooth, maintain meticulous oral hygiene
Critical Success Factor: The 15-Minute Rule
The most important technical consideration is keeping extraoral time under 15 minutes. Periodontal ligament cell viability decreases dramatically with prolonged drying. Have all materials and instruments ready before extraction begins.
Evidence-Based Outcomes
Success Rates from Recent Literature
Systematic reviews and meta-analyses published in 2024-2026 provide robust evidence for intentional reimplantation outcomes:
- Overall survival: 88-95% success rates reported across multiple studies
- Four-year survival: 82.8% when proper case selection and technique employed
- Long-term survival: 77-88% at 5+ years with appropriate follow-up
- Comparison to alternatives: Similar or superior to surgical endodontics for certain anatomical situations
Complications and Their Prevalence
Recent research identifies these potential complications:
- External root resorption: 11% prevalence overall
- Inflammatory resorption: Most common in first year post-treatment
- Replacement resorption (ankylosis): Less common but progressive when it occurs
- Root fracture during extraction: Higher risk with curved/flared roots—hence contraindication
- Re-infection: Rare when proper apical seal achieved with bioceramic materials
Monitoring Protocol
Follow-up schedule based on evidence-based recommendations:
- 1 week: Remove splint (if used), assess symptoms
- 3 months: Clinical exam and radiograph (check for early resorption)
- 6 months: Clinical exam and radiograph
- 12 months: Clinical exam, radiograph, CBCT if indicated
- Annual thereafter: Minimum 3-year follow-up recommended; most complications appear within first year
Patient Outcome in This Case
At 12-month recall:
- Complete resolution of pain and periapical symptoms
- Radiographic evidence of bone regeneration around apical region
- CBCT confirms healing of periapical lesion
- Tooth asymptomatic to percussion and palpation
- Normal function—patient reports no limitations
- No evidence of root resorption
Research Sources: These outcomes align with recent literature demonstrating 90% survival rates with proper case execution (PMC11621965). The shift from "last resort" to "adjunct modality" reflects improving outcomes and better understanding of critical success factors like the 15-minute extraoral time limit.
Key Takeaways
Clinical Decision-Making
- No longer a "last resort": Modern evidence supports intentional reimplantation as a predictable treatment option with 88-95% success when case selection is appropriate. It's a legitimate alternative to extraction/implant for preserving natural teeth.
- The 15-minute rule is critical: Research shows survival decreases significantly when extraoral time exceeds 15 minutes. Prepare all materials and instruments before extraction begins. Speed matters.
- Case selection determines success: Avoid teeth with severe root curvature, vertical fractures, or advanced periodontal disease. Choose cases where atraumatic extraction is feasible.
- Posts blocking access are ideal indications: When large posts or broken instruments make conventional retreatment impossible, intentional reimplantation provides direct access to apical anatomy.
- Bioceramic retrofills are standard of care: MTA and similar materials provide superior apical seals compared to older amalgam retrofills.
When to Consider This Technique
Intentional reimplantation is appropriate when:
- Nonsurgical retreatment is blocked by posts, separated instruments, or severe calcification
- Surgical access (apicoectomy) is impractical due to anatomy or adjacent structures
- Patient prefers tooth preservation over extraction/implant
- Root morphology allows atraumatic extraction (single-rooted or fused roots preferred)
- Adequate periodontal support and restorable crown structure exist
Evidence-Based Practice
Recent cross-sectional studies show 72.7% of endodontists now view intentional reimplantation as an adjunct modality rather than desperation treatment. The procedure is cost-effective, preserves natural tooth structure, and achieves success rates comparable to or exceeding traditional surgical endodontics for certain indications.
Bottom Line: Intentional reimplantation deserves a place in the modern endodontic treatment planning algorithm. With proper case selection, meticulous technique, and adherence to the 15-minute extraoral time limit, it offers patients a viable path to natural tooth preservation when conventional approaches fail.
Clinical Disclaimer: These cases are presented for educational purposes and published with appropriate patient consent. Patient identifying information has been removed in compliance with HIPAA regulations. Individual results may vary. All radiographic images and case descriptions represent actual patient treatment outcomes.
Procedures We Use for These Cases
The expertise demonstrated in these cases comes from mastering advanced endodontic procedures
Root Canal Retreatment in Torrance, CA
Failed root canal? Dr. Jason Phan specializes in root canal retreatment in Torrance using CBCT imaging and microscope technology to save teeth other dentists can't.
Learn moreEndodontic Surgery & Microsurgery in Torrance
Expert endodontic microsurgery and apicoectomy in Torrance. Minimally invasive surgical procedures using 25x microscopic magnification when traditional root canal treatment isn't enough.
Learn moreRelated Articles
Learn more about these treatments from Dr. Phan
 Surgery & Retreatment
Surgery & Retreatment Retreatment vs. Apicoectomy: Which Fixes a Failed Root Canal?
Failed root canal — should you redo it or go straight to surgery? Dr. Jason Phan compares retreatment vs. apicoectomy: when each works, success rates, costs, and recovery.
 Surgery & Retreatment
Surgery & Retreatment Failed Root Canal: Should You Try Retreatment or Get an Implant?
Your root canal didn't work — now what? Dr. Jason Phan compares retreatment vs. extraction and implant: success rates, costs, timelines, and how to decide which is right for your tooth.
 Root Canal
Root Canal Persistent Pain After Root Canal: Causes, Evidence, and When Retreatment Is Needed
A detailed clinical guide to understanding why pain persists after root canal treatment. Dr. Jason Phan covers odontogenic and nonodontogenic causes, diagnostic approaches, and evidence from current research.
 Surgery & Retreatment
Surgery & Retreatment Apicoectomy Explained: When Root Canal Isn't Enough
Sometimes a root canal isn't enough to save a tooth. Dr. Jason Phan explains what an apicoectomy is, when you need one, and what to expect during recovery.
 Surgery & Retreatment
Surgery & Retreatment Root Canal Retreatment: When Your First Root Canal Fails
Your root canal didn't work. Now what? Dr. Jason Phan explains why root canals fail, what retreatment involves, and when it's worth saving the tooth.
 Root Canal
Root Canal Root Canal Pain After Treatment: What's Normal and What's Not
Some discomfort after a root canal is normal, but how do you know if something is wrong? Dr. Jason Phan explains what to expect during recovery, warning signs to watch for, and when to call your endodontist.
Experience Matters in Complex Endodontics
When you refer patients to us, they benefit from decades of experience with the most challenging cases. We're here to help when routine endodontics isn't enough.
Mon-Fri: 8am-5pm | 23451 Madison St., Suite 210, Torrance, CA